Just because it doesn’t look dirty doesn’t mean it’s clean.
That’s always been true, of course. But the coronavirus pandemic is reinforcing this lesson in unspeakably tragic ways. A gleaming doorknob could well be coated with millions of SARS-CoV-2 viruses—a thousand of which could line up across the breadth of a human hair.
That same truth holds for the air around us. Look across the room. Unless a beam of sunlight happens to be catching dust, the air appears perfectly clear. But in fact, in a typical indoor space, it’s swarming with particles—millions and millions of them per cubic meter. Among the vast diversity of these particles include dust, pollen, fungal spores, pet dander and other allergens, vehicle exhaust and other pollution wafted in from outdoors, bacteria, and, yes, viruses. We’re breathing some combination of all that—all day, all night.
With the SARS-CoV-2 coronavirus that causes the disease called COVID-19, we’re now collectively up to speed on the fact that, when it comes to door knobs, mobile phones, keyboards, and other surfaces, “clean” and “disinfected” mean very different things. Fortunately, we also know what to do about it: regularly disinfect surfaces, frequently wash hands for 20 seconds, and assiduously avoid touching eyes, nose and mouth.
But how do we deal with the possibility of coronavirus in the air we breathe? How do you disinfect it?
First, droplets
This seemed a simple question in the early months of the coronavirus pandemic. Transmission was at first believed to be strictly animal-to-human (the World Health Organization shared that belief as late as mid-January). Once human transmission was established, the thought was that the disease transmitted through respiratory droplets from a symptomatic person’s coughing or sneezing.
The size of these respiratory droplets—greater than about 20 microns—gives gravity a decisive edge over air currents that keep smaller particles aloft, so the droplets fall quickly and, typically, within about three feet of the infected person. That was the basis for the U.S. Centers for Disease Control and Prevention’s recommendation to avoid close contact with others to prevent the disease’s spread (six feet separation being the standard, though a recent study says “turbulent gas clouds” from sneezes and such could extend as far as 27 feet).
Those same droplets, the reasoning went, were also the cause of touch-related infections. The droplets fell on a surface. Someone touched that surface and then touched their eyes, nose or mouth. COVID-19 soon had another notch in its belt. A New England Journal of Medicine laboratory study helped quantify the risk of such infection. Its findings: SARS-CoV-2 viruses remained viable (read: ready to infect) for three days on plastic, two days on stainless steel, and 24 hours on cardboard.
Now, aerosols
Airborne droplets and those that have landed but remain viable are still considered major COVID-19 transmitters. But now there’s increasing evidence that lingering airborne particles containing the coronavirus are also significant source of infection. Much of that evidence remains anecdotal, but that will probably change as scientists catch up to this rampaging epidemic. These airborne particles—aerosols smaller than about 5 microns across—are much smaller than droplets. Air currents countervail gravity’s pull much longer with aerosols, so these tiny particles can remain aloft for tens of minutes to hours, depending on the environment. These aerosols can, it appears, be spread by the basic acts of breathing and talking by those carrying COVID-19—even if they have no symptoms.
That’s likely what happened with the church choir group in Washington state. On March 10, sixty of them convened to sing together. None had cold or flu symptoms, and all were dispensed hand sanitizer on the way in. Save a bowl of clementine oranges that a few of them sampled, they avoided touching common surfaces, shaking hands, and hugging. Three weeks later, 45 of them tested positive for COVID-19 and three were dead.
“The outbreak has stunned county health officials, who have concluded that the virus was almost certainly transmitted through the air from one or more people without symptoms,” the Los Angeles Times reported.
Also, studies have shown coronaviruses similar to SARS-CoV-2—the original SARS of 2003 and MERS of 2012—to be “consistent with the hypothesis of an airborne transmission route,” as a January 2019 review concluded. The same report and others have described how aerosols of 5 microns and smaller have an alarming ability to penetrate deep into the lungs—which is where many serious cases of COVID-19 manifest.
These and other inputs as well as ongoing research led the National Academies of Sciences Standing Committee on Emerging Infectious Diseases and 21st Century Health Threats to tell the White House this on April 1: “Currently available research supports the possibility that [coronavirus] could spread via bioaerosols generated directly by patients’ exhalation.”
That talking and breathing may indeed spread the disease should come as no great surprise. That same New England Journal of Medicine study found that, when SARS-CoV-2 virus particles were suspended in a mist in their lab, they remained “viable and infectious” for three hours. In real-world conditions, they added, the aerosols would probably persist for 30 minutes.
Ben Cowling, an epidemiologist at the University of Hong Kong, put the droplet-versus-aerosol question in perspective. The distinction between droplets and aerosols is “unhelpful,” he told Nature, because “the particles that come out with virus can be a wide range of sizes. Very, very large ones right down to aerosols.”
A draft study posted by University of Nebraska researchers provided further evidence for respiratory aerosols as a coronavirus carrier. The researchers sampled air and various surfaces in 11 isolation rooms occupied by 13 COVID-19 patients. It found viral RNA in the air and essentially everywhere in the room (including under the bed) as well as in outside hallways—despite patients not having been observed to cough during air sampling. The highest concentration of viruses in a surface sample was found on an air-handling grate.
Clearing the air
Questions remain as to how many SARS-CoV-2 virions (virus particles) it takes to seed a new infection—and, by extension, how long and intense an exposure to such particles must be in different sorts of spaces. And perhaps the threat of tiny virus-laden particles lingering afloat and triggering new disease is overblown. But as we’ve seen so often, the coronavirus has turned what seemed like alarmism into wishful thinking in a matter of days.
The precautionary principle and plain old common sense demand that SARS-CoV-2 be considered infectious through aerosol particles. The question is how to deal with that.
Social distancing is the best insurance against such airborne exposure, but that’s not always possible. Hospitals, supermarkets, drug stores, and other critical businesses and services continue to require human contact. Those who visit those places return home to families and roommates.
Masks good enough to protect the uninfected from the infected (such as N95 masks in the United States; they have other names elsewhere) are in short supply and must be preserved for frontline medical personnel. Surgical masks and makeshift cotton masks can help minimize infection spread from an infected person, but are not at this time believed to provide much protection from infection. That leaves a solution that’s getting surprisingly little attention during this time of crisis: air filtration.
The CDC is among many who recognize value of clearing the air: they have published clear guidelines on the topic. In hospital settings as well as in areas where people can’t avoid common spaces—dispatch centers, waiting rooms, family rooms, bedrooms—a highly effective room air cleaner can trap pathogens as well as a wide range of harmful particles. Some of these are easier to capture than others. A quality HEPA filter does decent job with these larger particles such as pollen, asbestos, and general dust.
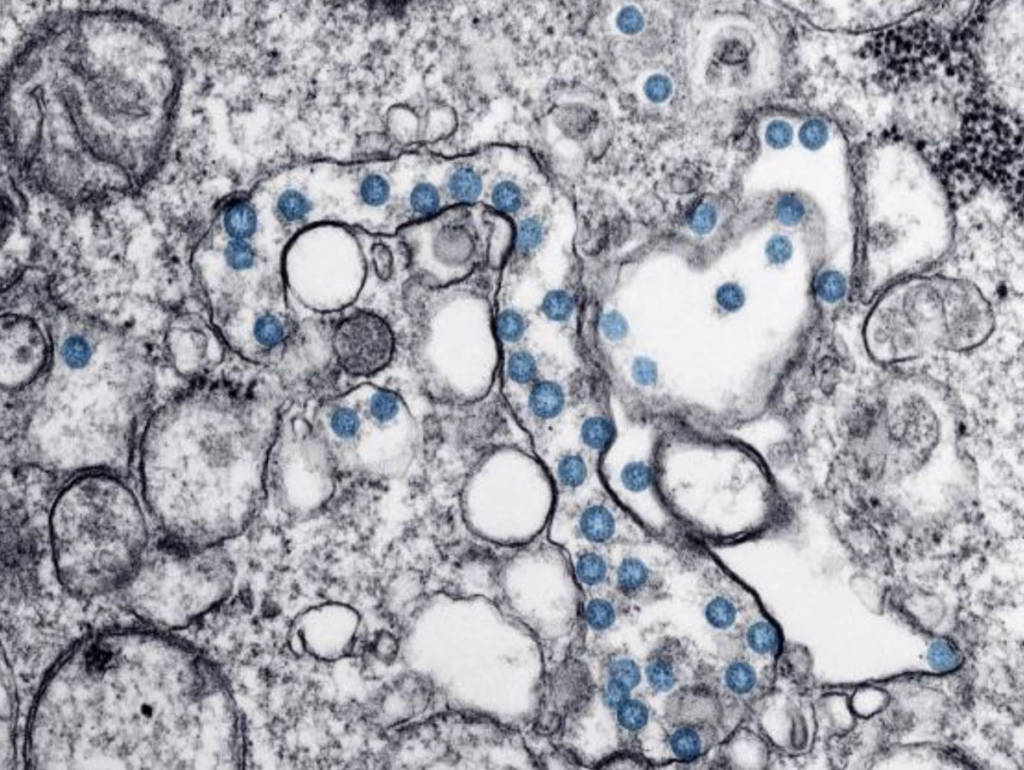
What is HEPA? It’s a standard of filtration that was developed in the 1940s during the Manhattan Project. The Department of Energy set this standard the removal of 99.97% particles that are as small as 0.3 microns. Zero-point-three microns is tiny: a red blood cell is more than 20 times wider. But the SARS-CoV-2 virions are smaller yet—around 0.1 micron across.
We know a lot more about filtration and particle size and behavior than we did 80 years ago, but the HEPA standard remains oddly unchanged. Many viruses are around the size of SARS-CoV-2. A standard that disregards the effectiveness of filtration below 0.3 microns—despite our knowledge of dangerous particles three times smaller—is inadequate today.
In fact, modern research found that particles right at that 0.1 micron size are actually the hardest to capture. Intuitively, larger particles are easier to net; less intuitively, particles smaller than 0.1 microns are also easier to capture thanks to Brownian motion, which explains how the tiniest particles are more likely to bounce off each other and leave the airflow so they hit the filter media at a higher rate. If you can capture the 0.1-micron particle, then, you’re capturing about everything else. But you must first be able to capture a 0.1-micron particle. HEPA doesn’t require that. Either an updated HEPA or a new, tighter standard should.
Until that happens, hospitals, healthcare providers and homeowners alike should look for an air cleaner that effectively removes particles down to 0.1 microns in size—again, the toughest to snare and the size of many viruses SARS-CoV-2 virions. Use of such an air cleaner in areas where people share common air can remove viruses and virus-laden aerosols that could otherwise hover in a room hours, risking infection to caregivers and family who enter.
Unfiltered air can look clean. It isn’t. In normal times, the air around us can—and does—cause serious health problems, contributing to infectious disease, allergies and asthma, cardiopulmonary disease and more. These are not normal times. Truly clean air can save lives by protecting us from COVID-19 infection and, by both flattening the curve and by providing a safer working environment, keeping doctors, nurses and others working in hospitals healthy at a time when we need them most. An effective room air cleaner will not reduce the obligation to continue with those behaviors that you can control, especially responsible social distancing and the frequent washing of hands. But an air cleaner does address one area that we cannot control individually—the quality of the air in places shared by the healthy and unhealthy alike.
